The Courage Awards annually recognize a person and their family who has been diagnosed with an Autism Spectrum Disorder and demonstrates great character and perseverance in living with the challenges of this disorder.
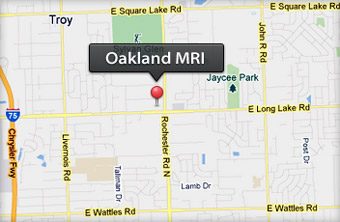
There will be two awards presented. One will recognize an individual, sponsored by Susan V. Swider and Oakland MRI. The other will acknowledge the individual and their family, sponsored by Dr. Lucia Zamorano and Michigan Brain & Spine Surgery Center. The award will be presented to the winners at the annual Ted Lindsay Foundation Celebrity Golf Outing on Monday September 12, 2022 at Detroit Golf Club, Detroit, MI.
Ted Lindsay Foundation support research and educational programs focusing on the cause and management of Autism Spectrum Disorders.


 The use of MRI to determine heart function has been slow to catch on, but a study from Duke Health researchers shows that stress cardiac MRI not only diagnoses disease but can also predict which cases are potentially fatal. Results from a large, multi-center study suggest that Cardiac Magnetic Resonance, or CMR, has potential as a non-invasive, non-toxic alternative to stress echocardiograms, catheterizations and stress nuclear exams in identifying the severity of coronary artery disease. The study appears online Feb. 8 in JAMA Cardiology. “We’ve known for some time that CMR is effective at diagnosing coronary artery disease, but it’s still not commonly used and represents less than one percent of stress tests used in this country,” said senior author Robert Judd, Ph.D., co-director of the Duke Cardiovascular Magnetic Resonance Center.
The use of MRI to determine heart function has been slow to catch on, but a study from Duke Health researchers shows that stress cardiac MRI not only diagnoses disease but can also predict which cases are potentially fatal. Results from a large, multi-center study suggest that Cardiac Magnetic Resonance, or CMR, has potential as a non-invasive, non-toxic alternative to stress echocardiograms, catheterizations and stress nuclear exams in identifying the severity of coronary artery disease. The study appears online Feb. 8 in JAMA Cardiology. “We’ve known for some time that CMR is effective at diagnosing coronary artery disease, but it’s still not commonly used and represents less than one percent of stress tests used in this country,” said senior author Robert Judd, Ph.D., co-director of the Duke Cardiovascular Magnetic Resonance Center. In 1983, Robert “Bob” Kagan, a 36-year-old pathologist, set out on foot from Holy Cross Hospital in Ft. Lauderdale, Florida, looking for a place to birth an industry. He’d find it in a McDonald’s, which would become one of America’s first outpatient MRI centers.
In 1983, Robert “Bob” Kagan, a 36-year-old pathologist, set out on foot from Holy Cross Hospital in Ft. Lauderdale, Florida, looking for a place to birth an industry. He’d find it in a McDonald’s, which would become one of America’s first outpatient MRI centers. Millions of magnetic resonance imaging (MRI) scans are performed each year to diagnose health conditions and perform biomedical research. The different tissues in our bodies react to magnetic fields in varied ways, allowing images of our anatomy to be generated. But there are limits to the resolution of these images—generally, doctors can see details of organs as small as a half millimeter in size but not much smaller. Based on what the doctors see, they try to infer what is happening to cells in the tissue.
Millions of magnetic resonance imaging (MRI) scans are performed each year to diagnose health conditions and perform biomedical research. The different tissues in our bodies react to magnetic fields in varied ways, allowing images of our anatomy to be generated. But there are limits to the resolution of these images—generally, doctors can see details of organs as small as a half millimeter in size but not much smaller. Based on what the doctors see, they try to infer what is happening to cells in the tissue.
 Adding screening mammography to annual screening MR imaging for women at high risk for breast cancer does not increase cancer detection rates, according to a study published in Radiology.
Adding screening mammography to annual screening MR imaging for women at high risk for breast cancer does not increase cancer detection rates, according to a study published in Radiology.